Expand all
Collapse all
Overview
The thyroid gland is a butterfly-shaped gland in the neck, containing a central isthmus and two lobes on either side of the trachea. It is an endocrine organ which plays a role in regulating the body’s metabolism. Hormones triiodothyronine (T3) and thyroxine (T4) are released by the gland and T4 is converted to T3 via body tissues. T3 and to a much lesser extent T4 act via receptors to initiate metabolic pathways. This includes the following:
- basal metabolic rate
- gluconeogenesis
- glycogenolysis
- protein synthesis
- lipogenesis (Longmore et al, 2014; NHS, 2021; British Thyroid Foundation, 2022)
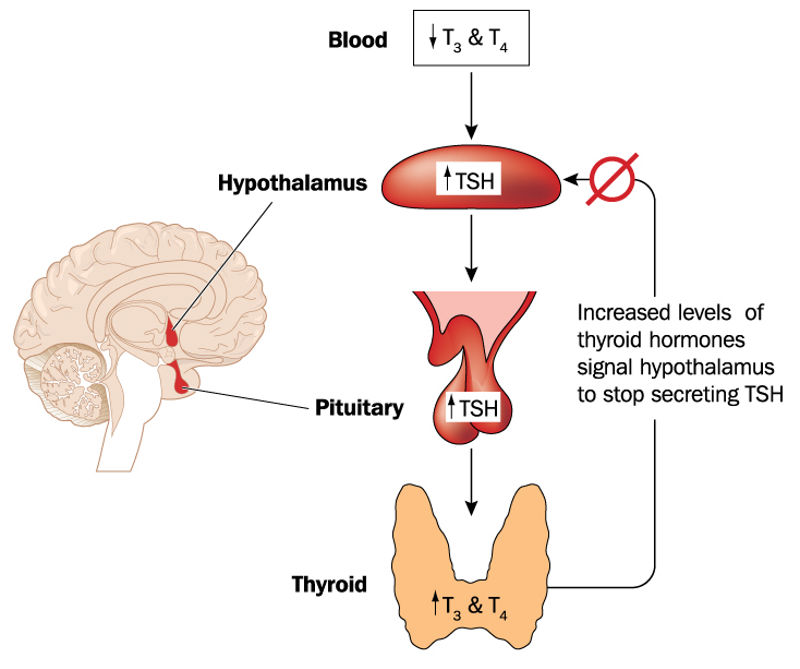
The hypothalamus releases thyrotropin-releasing hormone (TRH), stimulating the anterior pituitary gland to release thyroid-stimulating hormone (TSH). TSH stimulates the thyroid gland
To view the rest of this content login below; or read sample articles.
Symptoms
The symptoms of thyroid disorders differ depending on whether the patient has hypothyroidism or hyperthyroidism.
Hypothyroidism symptoms may include:
- lethargy
- cold intolerance
- weight gain
- constipation
- depression and low mood
- memory problems and brain fog
- muscle aches and cramps
- dry skin and hair
- hair loss
- hoarse voice
- brittle nails
- loss of libido
- carpal tunnel syndrome symptoms
- change in menstrual cycle (Longmore et al, 2014; NHS, 2021)
Hyperthyroidism symptoms (thyrotoxicosis) may include:
- irritability
- nervousness and anxiety
- labile emotions
- heat intolerance
- poor sleep
- neck swelling (from enlarged thyroid gland)
- palpitations
- sweats
- tremor
- weight loss (Longmore et al, 2014; NHS, 2021)
To view the rest of this content login below; or read sample articles.
Aetiology
Hypothyroidism
The prevalence of diagnosed hypothyroidism in the UK is approximately 3% of the UK population.
When the deficiency in T3 and T4 is caused by the thyroid gland directly this is known as a primary cause. These include:
- autoimmune thyroid disease – Hashimoto’s thyroiditis is the most common type and is more frequently diagnosed in women aged 60–70 years.
- iodine deficiency
- prior treatment for thyroid cancer or hyperthyroidism
- drugs – including amiodarone and lithium (British Thyroid Foundation, 2021; National Institute for Health and Care Excellence (NICE), 2021)
Secondary causes are much rarer and are the result of a pituitary or hypothalamic disorder.
Congenital hypothyroidism is a form of hypothyroidism that affects infants at birth and is tested for routinely. One in every 2000 to 3000 infants has congenital hypothyroidism in the UK (British Thyroid Foundation, 2018).
Hyperthyroidism
Hyperthyroidism has approximately a 2% prevalence in the UK.
To view the rest of this content login below; or read sample articles.
Diagnosis
Thyroid conditions should be suspected based on history of symptoms and risk factors (Table 1).
| Table 1. Signs of hyper- and hypothyroidism | |
| Hyperthyroidism | Hypothyroidism |
| Rapid-onset malaise, fever and thyroid pain (suggesting thyroiditis) |
Weakness and myalgia |
| Weight loss | Weight gain |
| Anxiety, tremor and sweating | Impaired concentration and memory |
| Diffuse alopecia | Dry skin and hair loss, notably loss of lateral eyebrows |
| Peripheral oedema | Oedema, particularly swelling of eyelids |
| Breathlessness and hoarse voice | Hoarse voice |
| Goitre | Goitre |
| Fast pulse or irregular pulse (atrial fibrillation) | Slow pulse |
| Palmar erythema | Raised diastolic blood pressure |
| Muscle wasting and hyper-reflexia | Delayed relaxation of deep tendon reflexes |
| Vitiligo | Features of other autoimmune disease |
| Splenomegaly | Features of pituitary disease- such as recurrent headache, double vision or visual field defect, skin depigmentation |
| Lymphadenopathy | |
| Gynaecomastia | |
| Features of Graves’- including clubbing of distal fingers and toes, pigmented and thickened skin of the shins and changes in appearance of eyes | |
To view the rest of this content login below; or read sample articles.
Management and treatment
Primary hypothyroidism
Levothyroxine is a synthetic version of T4 and is the main treatment. Doses are titrated according to TSH levels, which should be maintained within the reference range. This medication should be initiated with caution in patients who are pregnant, diabetic, older people or have a history of cardiovascular disease (NICE, 2019; NHS, 2021; NICE, 2021).
Subclinical hypothyroidism
Levothyroxine treatment is considered where there are clinical features of hypothyroidism, consistently raised levels of TSH, previous radioactive iodine treatment or surgery or raised thyroid autoantibodies (NICE, 2019; 2021).
Overt hyperthyroidism
Patients with overt hyperthyroidism should be admitted to hospital if they have any features of thyrotoxic crisis, including fever, tachycardia, agitation, hypothermia, hypertension, atrial fibrillation, confusion and features of heart failure.
If there are no features of a thyrotoxic crisis, the patient is referred to an endocrinologist for consideration of the following treatments:
- Beta
To view the rest of this content login below; or read sample articles.
Resources
References
British Thyroid Foundation. Congenital Hypothyroidism. 2018. https://www.btf-thyroid.org/congenital-hypothyroidism (accessed 17 February 2023)
British Thyroid Foundation. Hypothyroidism. 2021. https://www.btf-thyroid.org/hypothyroidism-leaflet (accessed 17 February 2023)
British Thyroid Foundation. Your thyroid gland. 2022. https://www.btf-thyroid.org/what-is-thyroid-disorder (accessed 17 February 2023)
Cancer Research UK. Thyroid Cancer. 2021. https://www.cancerresearchuk.org/about-cancer/thyroid-cancer (accessed 17 February 2023)
Longmore M, Wilkinson I, Baldwin A, Wallin E. Oxford Handbook of Clinical Medicine. (9th edn). Oxford: Oxford University Press; 2014
NHS. Overactive Thyroid, Hyperthyroidism. 2019. https://www.nhs.uk/conditions/overactive-thyroid-hyperthyroidism/ (accessed 17 February 2023)
NHS. Thyroid Cancer. 2019. https://www.nhs.uk/conditions/thyroid-cancer/ (accessed 17 February 2023)
NHS. Underactive Thyroid, Hypothyroidism. 2021. https://www.nhs.uk/conditions/underactive-thyroid-hypothyroidism/ (accessed 17 February 2023)
NHS. Levothyroxine. 2021. https://www.nhs.uk/medicines/levothyroxine (accessed 17 February 2023)
National Institute for health and Care Excellence. Hyperthyroidism. 2021. https://cks.nice.org.uk/topics/hyperthyroidism/ (accessed 17 February 2023)
National Institute for health and Care Excellence. Hypothyroidism. 2021.
https://cks.nice.org.uk/topics/hypothyroidism/ (accessed 17 February 2023)
National Institute for health and Care Excellence. Thyroid Disease, Assessment and Management. 2019. https://www.nice.org.uk/guidance/ng145/chapter/Recommendations#managing-and-monitoring-subclinical-hyperthyroidism (accessed 17 February 2023)
To view the rest of this content login below; or read sample articles.